Overview
In men with prostate cancer, radiation can be used instead of surgery, or it may be used after surgery to destroy any cancer cells that may remain in the area. In advanced stages of prostate cancer, it may be given to relieve pain or other problems. Radiation therapy can be given in a variety of ways. The two most common ways that radiation therapy can be delivered are through external beam radiation therapy and brachytherapy.
External Beam Radiation Therapy for Prostate Cancer
External beam radiation therapy (EBRT) for prostate cancer is given on an outpatient basis, 5 days a week, for approximately 8 to 9 weeks. EBRT begins with a planning session, or simulation, where body position is determined and a scan is performed so that the target can be precisely determined, the beam alignment planed and the dose prescribed. About a week after the simulation, the treatment plan will be complete. Patients return and lie on a table and are treated with radiation as the machine moves around their body in a wide circle. The actual area of the pelvis receiving radiation treatment may be large or small, depending on the features of the cancer. Radiation can be delivered specifically to the prostate gland (prostate only radiation) or encompass the surrounding pelvic lymph nodes in addition to the prostate gland (whole pelvic radiation). Sometimes patients receive a second planning session partway through the treatment to focus the beam even further where additional dose is needed most.
Although normal cells have the ability to recover, the goal of radiation therapy is to maximize the dose to the prostate while minimizing exposure to the bladder and rectum (and, therefore, minimizing the risks and severity of side effects). The challenge is to conform the radiation delivery as precisely as possible to the location, shape, size and orientation of the prostate. Over the years, EBRT has advanced to offer ever-better targeting and conformance in order to shrink and destroy the prostate cancer cells:
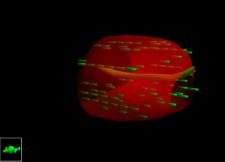
- Three-dimensional conformal radiation therapy (3DCRT) – Using three-dimensional imaging (computed tomography, or "CAT scan"), our radiation oncologists and physicists can devise a treatment based on—and customized to—a prostate's shape, size, location and proximity to other normal anatomic organs and structures.
- Intensity-modulated radiation therapy (IMRT) – Powerful computer software lets us plot treatment angles and varied beam intensities based on the true size, shape, density, location and orientation of the prostate. Pairs of tungsten "leaves" extend into and retract out of the radiation beam, shaping smaller beams and modulating radiation intensity for even greater 3D conformance. This effectively "wraps" the high dose region tightly around the target.
- RapidArc™ – an advanced form of IMRT, now routinely utilized by our radiation oncologist Dr. Alden at USLV, the RapidArc Linear Accelerator radiation therapy technology allows very complex treatments to be delivered in ten minutes or less, precisely to the targeted area, sparing healthy tissue, in contrast to the earlier technologies which required a 15- to 25-minute treatment to achieve the same results. RapidArc permits the entire radiation dose to be administered to the entire tumor with just one single rotation of the machine around the patient. This means that there is less chance of inadvertent patient or organ movement during treatment, so it reduces chances of having targeting errors, and potentially less side effects. Most importantly, RapidArc can achieve the same high cure rates for urologic cancers as the previous delivery systems.
- Image-guided radiation therapy (IGRT) – Because the cancer site (and normal structures) can move between planning and treatment and day to day, it is customary in older technology to expand the treatment region by a "margin" to allow for this movement. The advancement with IGRT, is that we use imaging technology to precisely locate the target are at the moment before each treatment, which improves accuracy, reduces the treatment margins and further minimizes exposure to normal tissue. Ultimately, this prevents excess high dose radiation exposure to your healthy tissue, and minimizes the chance of side effects.
Interstitial Brachytherapy
 Internal radiation is known by a number of names: "interstitial brachytherapy," "seeds," or "implantation." These terms refer to treatment where radioactive material is placed directly into the prostate gland. For prostate cancer, the most common method of interstitial brachytherapy is permanent implantation of radioactive Iodine seeds into the prostate gland. It is performed by inserting a needle through the perineum into the prostate gland. The perineum is the area of skin between the scrotum and the anus. The implantation procedure is performed in the operating room while the patient is asleep under general anesthesia. An imaging device known as an ultrasound is inserted into the rectum to visualize and guide placement of the seeds. The patient is typically discharged home later in the day with a bladder catheter for a few days, which will be removed in the doctor's office. Following the procedure, patients will experience some pain or aching in the perineum and may experience burning or discomfort during urination. Occasionally, a patient will be unable to urinate, and may require a bladder catheter for several days or weeks to allow passage of urine. Also infrequently, a patient may lose control of urine, and this seems to occur more often in men who have had a previous transurethral resection of the prostate (TURP). Approximately 30% to 50% of men lose their ability to get an erection following placement of brachytherapy seeds, but this make take several years to occur. After the procedure, the patient will temporarily emit a small amount of radiation from the seeds. Though this amount is generally not dangerous to most other people, doctors will usually advise patients to avoid close contact with children under the age of 19 or pregnant women for several months afterward. Because implant radiation focuses the radiation closely around the prostate, this form of radiation works best in patients with early stage prostate cancer. However, if the prostate-specific antigen (PSA) level or Gleason score are high, EBRT may be added or recommended instead in order to improve results. Also, seed implantation does not work as well in patients who have had prior transurethral resection of the prostate (TURP) or prior prostate infections, or in patients with larger size prostate glands, or who have many urinary symptoms.
Internal radiation is known by a number of names: "interstitial brachytherapy," "seeds," or "implantation." These terms refer to treatment where radioactive material is placed directly into the prostate gland. For prostate cancer, the most common method of interstitial brachytherapy is permanent implantation of radioactive Iodine seeds into the prostate gland. It is performed by inserting a needle through the perineum into the prostate gland. The perineum is the area of skin between the scrotum and the anus. The implantation procedure is performed in the operating room while the patient is asleep under general anesthesia. An imaging device known as an ultrasound is inserted into the rectum to visualize and guide placement of the seeds. The patient is typically discharged home later in the day with a bladder catheter for a few days, which will be removed in the doctor's office. Following the procedure, patients will experience some pain or aching in the perineum and may experience burning or discomfort during urination. Occasionally, a patient will be unable to urinate, and may require a bladder catheter for several days or weeks to allow passage of urine. Also infrequently, a patient may lose control of urine, and this seems to occur more often in men who have had a previous transurethral resection of the prostate (TURP). Approximately 30% to 50% of men lose their ability to get an erection following placement of brachytherapy seeds, but this make take several years to occur. After the procedure, the patient will temporarily emit a small amount of radiation from the seeds. Though this amount is generally not dangerous to most other people, doctors will usually advise patients to avoid close contact with children under the age of 19 or pregnant women for several months afterward. Because implant radiation focuses the radiation closely around the prostate, this form of radiation works best in patients with early stage prostate cancer. However, if the prostate-specific antigen (PSA) level or Gleason score are high, EBRT may be added or recommended instead in order to improve results. Also, seed implantation does not work as well in patients who have had prior transurethral resection of the prostate (TURP) or prior prostate infections, or in patients with larger size prostate glands, or who have many urinary symptoms.
External Beam Radiation or Interstitial Brachytherapy or Surgery?
The decision to undergo EBRT, brachtherapy or radical prostatectomy can be difficult. This is because these treatment strategies have never been directly compared in well-designed clinical studies. The choice of radiation versus prostatectomy is often based on weighing the age and health status of the patient, possible complications of treatment and the relative inconvenience of the treatments. It is important to be seen by more than one physician to determine the likely treatment outcome associated with the various options available in your community. Questions you may wish to ask your physicians include:
- What are the chances of this treatment curing the cancer?
- What is the risk of impotence and incontinence?
- What are the other possible complications from this treatment?
The results of a review of 1,872 patients with early stage prostate cancer who were treated with either radical prostatectomy, EBRT, or brachytherapy at the University of Pennsylvania Medical Center and Harvard Medical School were reported in 1998. High-risk patients (patients least likely to have cancer confined to the prostate) treated with brachytherapy were over twice as likely to experience cancer recurrence within 3-4 years of treatment compared to patients treated with radical prostatectomy or EBRT. Approximately 60% of patients treated with prostatectomy or EBRT survived without evidence of cancer recurrence, compared to approximately 35% of patients treated with implants. Patients at low risk (those with a high chance of having cancer confined to the prostate) did equally well 3-4 years from treatment whether they received EBRT, radical prostatectomy, or radiation using brachtherapy.
In summary, for patients with low-risk, early stage prostate cancer, treatment with radical prostatectomy, EBRT, or implants appears equivalent. In patients with higher-risk disease, however, treatment with EBRT or radical prostatectomy may be superior to implants. It is important to realize that patients with low-risk disease have not been followed long enough to conclude there is no difference between these three therapeutic approaches. Lastly, this was not a direct comparison of three different treatment approaches in a controlled fashion, and a number of other factors could influence the outcome of the various treatment options. Hopefully, the results of this clinical analysis will help men and their families make more informed decisions as they sort through the maze of prostate cancer treatment options. However, the most current, up to date data on the treatment choices for prostate cancer can be accessed through some of the websites listed here on our Patient Education page.
Side Effects from Radiation Therapy
Although patients do not usually feel anything while receiving a single radiation treatment, the effects of radiation gradually build up over time. Most men have few side effects; however, some patients experience fatigue as treatment continues. Loose stools or diarrhea may also temporarily occur. Urination may become more frequent , urgent or uncomfortable. Some patients may experience loss of pubic hair or irritation of the skin, particularly between the buttocks. Long term, men receiving radiation therapy for prostate cancer can lose their ability to get an erection, see a drop of blood in their stool, or have a minor change in urinary habits. The risk of impotence is approximately 25% to 50% depending on other factors also such as prior ED or other concurrent medical conditions.
What if Cancer Returns After Radiation Therapy?
In some patients, prostate cancer cells can regenerate themselves in the prostate or escape the prostate gland and spread to other areas of the body. If the cancer is still in the prostate, salvage treatment such as cryoablation of the prostate can be given. In advance cases, hormonal and chemotherapy are needed. Sometimes prostate cancer cells spread to the spine and pelvis/hip bones of the body and can cause pain and other problems. This pain can often be relieved with EBRT directed to the affected bones. The side effects of radiation therapy for relief of bone pain depends on the area of the body being treated and are commonly very mild.
Is Radiation Necessary after Prostatectomy?
Radiation therapy may be recommended to patients following radical prostatectomy if they are found to have cancer cells invading the seminal vesicles or the margins of the surgical specimen, or outside the capsule of the prostate, or if the PSA remains persistently elevated, or the PSA returns to normal and then begins rising again. Patients with cancer involving the seminal vesicles or surgical margins with a persistently elevated or a rising PSA have evidence that some prostate cancer cells were not removed by surgery. For some patients, the remaining cancer will be confined to an area near the prostate gland. For other patients, the cancer may have spread to more distant locations in the body. Your doctor will help you decide how best to salvage this situation. Patients with high Gleason scores, more advanced stages and higher PSA levels are more likely to have cancer recurrence following surgery or radiation than those with lower Gleason scores and lower PSA levels.
Strategies to Improve Treatment
The progress that has been made in the treatment of prostate cancer has resulted from improved development of radiation treatments and surgical techniques and participation in clinical trials. Future progress in the treatment of prostate cancer will result from continued participation in appropriate clinical trials. Currently, there are several areas of active exploration aimed at improving radiation treatment of prostate cancer.
At USLV, we utilize IMRT, IGRT, and RapidArc technologies together with careful patient preparation to achieve the best outcomes.
Combination Radiation and Hormonal Therapy
Some radiation oncologists are combining EBRT and hormonal therapy for patients with higher-risk stage II or III cancers. The purpose of the EBRT is to treat the prostate and surrounding tissues and lymph nodes where cancer cells may have spread, while the hormonal agents serve to weaken these cancer cells by starving them of their growth stimulation factors.
Whole Pelvic Radiation Therapy
Because certain patients are at higher risk of cancer involving the pelvic lymph nodes, some doctors have advocated expanding the radiation field to include the pelvic lymph nodes. This is referred to as whole pelvic radiation therapy (WPRT). Some, but not all, comparisons of WPRT to prostate only radiation therapy have demonstrated that WPRT may improve survival, and is associated with only a few more side effects than radiation to the prostate only. Many doctors believe, however, that if cancer has spread to the pelvic lymph nodes, it has probably spread elsewhere in the body and expanding the radiation field will be of little benefit. Efforts to improve treatment might be better focused on systemic treatment approaches in addition to local treatment with radiation. Doctors in the United States are currently conducting a clinical study comparing WPRT to prostate only radiation.
Newer Radiation Machines
Most EBRT uses high energy x-rays to kill cancer cells. Some radiation oncology centers use different types of radiation which require special machines to generate. These are different types of radiation, such as protons or neutrons. Combining protons or neutrons with conventional x-rays is one method of radiation therapy being currently used, but has not been as thoroughly evaluated in clinical trials and has never been shown to have superior results compared to the more current and widely available radiation systems described above.
